Don’t expect it to mimic telemedicine.
Telemedicine is catching on among physicians. How about teledentistry? In February, the American Medical Association reported that physician adoption of televisits and virtual visits (including audio/video connections with patients) doubled, from 14 percent in 2016 to 28 percent in 2019. In addition, physician adoption of remote monitoring increased from 13 percent in 2016 to 22 percent in 2019.
On the other hand, it has been about two years since teledentistry codes – D9995 and D9996 – were added to the code set. But data on its usage is hard to come by.
Chances are, teledentistry will take a very different course among dental practitioners than telemedicine has among physicians. Some of that is due to the nature of the beast(s). Dentistry is, after all, a hands-on business. But regulatory policy – and politics – is playing a role too.
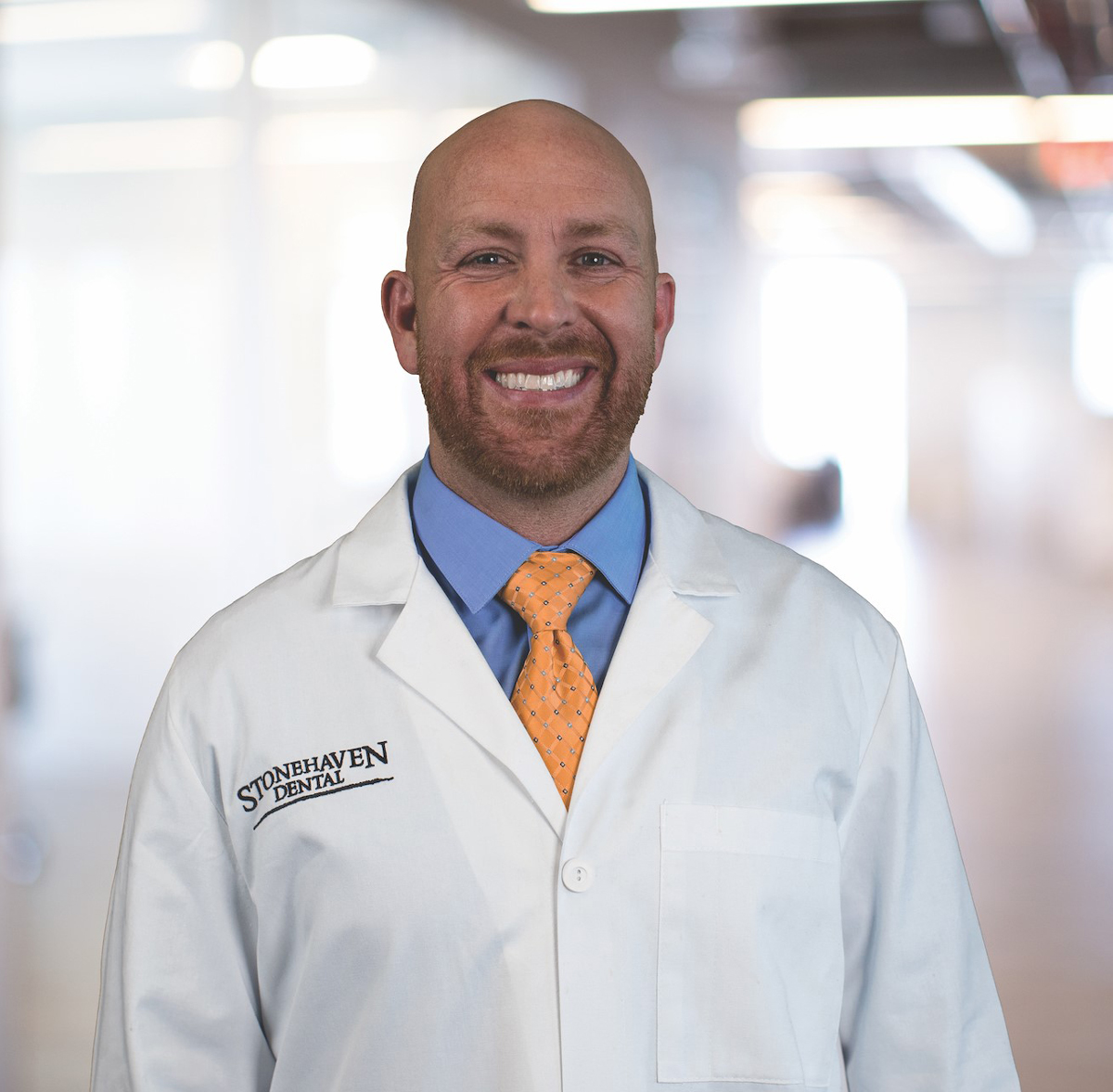
“There is a fundamental challenge with teledentistry compared to telemedicine,” says Eric Tobler, DMD, regional president, Stonehaven Dental in Northern Utah, and national director of clinical affairs for Mortenson Dental Partners. “In medicine, a large percentage of diagnoses can be entirely treated with medication.” That’s not the case in dentistry. “Most of what we do as dentists requires some physical treatment.”
What’s more, today’s medical practitioners rely on technologies that remotely monitor and assess their patients’ blood sugar levels, heart rates and blood pressure, he points out. Similar technologies don’t exist in dentistry.
But clinical and technological considerations are only part of the reason teledentistry faces a different future than telemedicine.
“Many people see teledentistry as something that may work, but there are just as many obstacles,” says Dr. Tobler. The state dental board’s role is to protect the standard of care and promote safety and access to care within their states – not to drive innovation, he says. “Until teledentistry business models can answer questions about comprehensive care and diagnosis, I think they will struggle with state board approval.”
A second challenge associated with state dental board approval is the fragmentation and inconsistency from state to state, he adds. State boards struggle to agree on “common sense” measures, such as a National Clinical Board Examination, he says. And “from state to state, we can’t agree on how to delineate responsibilities among dentists, hygienists and dental assistants. So, to expect national acceptance of something as nuanced and challenging as teledentistry is unreasonable in our current environment.”
Real-life applications
Despite the roadblocks, some doctors are using basic teledentistry to treat patients in emergency situations or follow-up care, says Dr. Tobler. “When I am taking emergency calls, I always encourage patients to take a picture of their issue with a cellphone and send it to me. This often allows me to diagnose something quickly as either nothing to worry about or something serious that requires a face-to-face appointment. I also find it useful for doctor-to-doctor communications.”
Teledentistry can also play a role in cosmetic consultations, he adds.
“A patient can send in pictures of their teeth and smile to give the provider a sense of what it would take to cosmetically fix their smile. The patient will then have a preliminary idea of what their price and treatment options are as they go into their face-to-face consultation. I see this as room for growth for teledentistry.”
Under current circumstances, teledentistry may be problematic, he says. “However, in our ever-increasingly connected world, it is not unreasonable to think that additional opportunities will present themselves,” he says.
“Teledentistry represents an opportunity to serve patients better and drive more patients to the practice. It also fosters relationship-building with the patient.”
Sidebar 1 –
A definition of terms
The term “teledentistry” refers to the delivery of patient care and education using, but not limited to, the following modalities:
- Live video (synchronous): Live, two-way interaction between a person (patient, caregiver, or provider) and a provider using audiovisual telecommunications technology.
- Store-and-forward (asynchronous): Transmission of recorded health information (for example, radiographs, photographs, video, digital impressions and photomicrographs of patients) through a secure electronic communications system to a practitioner, who uses the information to evaluate a patient’s condition or render a service outside of a real-time or live interaction.
- Remote patient monitoring (RPM): Personal health and medical data collection from an individual in one location via electronic communication technologies, which is transmitted to a provider in a different location for use in care and related support of care.
- Mobile health (mHealth): Health care and public health practice and education supported by mobile communication devices such as cell phones, tablet computers, and personal digital assistants (PDA).
Source: ADA Policy on Teledentistry, American Dental Association, 2015, www.ada.org/en/about-the-ada/ada-positions-policies-and-statements/statement-on-teledentistry
Sidebar 2 –
Patients’ rights
Per the 2015 ADA Policy on Teledentistry, dental patients whose care is rendered or coordinated using teledentistry modalities have the right to expect:
- That any dentist delivering services using teledentistry technologies will be licensed in the state where the patient receives services, or be providing these services as otherwise authorized by that state’s dental board.
- Access to the licensure and board certification qualifications of the oral health care practitioner who is providing the care in advance of the visit.
- That they will be informed about the identity of the providers collecting or evaluating their information or providing treatment, and of any costs they will be responsible for in advance of the delivery of services.
- That the provision of services using teledentistry technologies will be properly documented and the records and documentation collected will be provided to the patient upon their request.
- That services provided using teledentistry technologies and methods include care coordination as a part of a dental home and that the patient’s records be made available to any entity that is serving as the patient’s dental home.
- That the delivery of services using teledentistry technologies are performed in accordance with applicable laws and regulations addressing the privacy and security of patients’ private health information.
To see additional patients’ rights, see the 2015 ADA Policy on Teledentistry, www.ada.org/en/about-the-ada/ada-positions-policies-and-statements/statement-on-teledentistry
Sidebar 3 –
Putting a price on teledentistry
Chances are, teledentistry will not have the same impact on the dental profession as telemedicine already has had on physicians. After all, pain can rarely be diagnosed without an appointment. And how many remote sites – such as homes – are equipped with intraoral cameras?
That being the case, it’s no surprise that teledentistry isn’t top of mind for dental insurers. And that’s not likely to change anytime soon, says Mike Cole, vice president of insurance plan management for Dental Care Alliance.
“To dental insurers, teledentistry is simply an exam,” says Cole, who oversees a team of 16 people. “It’s very low cost and very easy to approve. However, there are limits on exams, and that’s the downside of teledentistry. If a teledentist bills for an exam and the patient comes to the office for a more thorough exam, the second one is not covered.”
In 2017, the American Dental Association introduced two CDT codes for teledentistry – D9995 (synchronous) and D9996 (asynchronous). But the codes have had little impact on dental practitioners, says Cole.
“We aren’t clear on when we would use these codes and, to be honest, why we would use them,” he says. The codes may be useful if a practitioner in the field – e.g., a hygienist – calls in to the dentist. “At least, in that case, you have a clinician ‘examining’ the patient. But outreach is different than pure teledentistry, in my opinion.”
Medicaid hasn’t proven to be much of a factor in teledentistry either, he says. “Medicaid is predominantly for children or those under the age of 21, and they need to be seen by a dentist for a comprehensive exam.
“In my opinion, teledentistry is not the way to reach Medicaid patients. Mobile units and health departments are far more effective.”
Cole, self-admittedly has “been around for a while,” including 21 years at DCA. “I’ve personally observed many changes in the industry. I do not believe teledentistry will ever be in a similar position as telemedicine.
“Dentists receive calls from patients after hours, and the answer is always, ‘Please come in first thing in the morning so you can be seen,’” he says. “We know that, at a minimum, we’ll bill for a 0140 problem-focused exam and radiographs to diagnose the complaint.
“That’s not going to change.”